Introduction
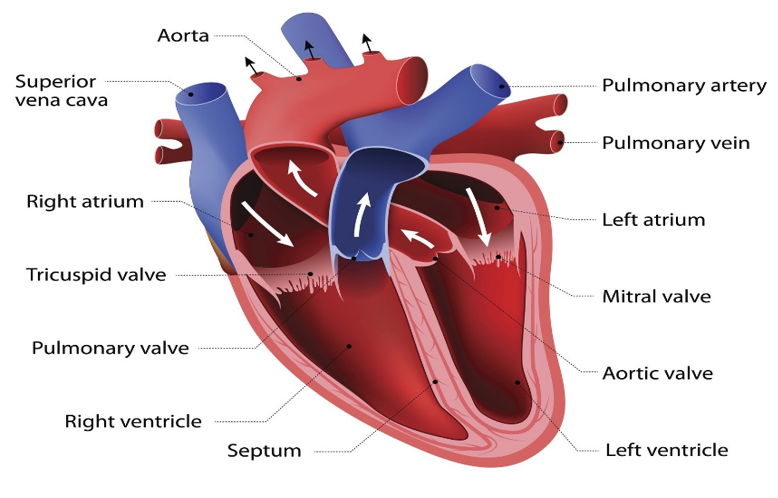
Congenital heart disease refers to any anatomical defect in the heart or major blood vessels present in children at birth. CHD (congenital heart disease) occurs in round about 1% of live births in developed countries.1, 2, 3 The incidence of congenital heart disease at birth is variable, incidence figures use to range between 5-8/1000 live births before the introduction of echocardiography but due to better diagnosis in today’s era many more milder forms are being detected, so the current estimates range from 8-12/1000 live births. 4 In developing countries due to poor resources, delayed diagnosis and surgery for CHD leads to a vicious cycle of congestive heart failure and respiratory infections 5, resulting in a high prevalence of preoperative malnutrition in patients with CHD. 6 Mechanisms for malnutrition in CHD has multiple factors including associated genetic anomalies and syndromes, inadequate nutrition due to improper feeding techniques and poorer nutritional absorption from digestive tract due to congestive heart failure, increased myocardial and respiratory neurohumoral functions in CHD cases. Chronic heart failure and hypoxia in CHD disturbs the cellular metabolism and growth, while repeated chest infections increase the metabolic requirements. 7 In children with congenital heart disease, the hemodynamic change provoke certain changes in nutritional status, brings about growth deficit and complicates the post-surgical survival. These deficiencies lead to increased morbidity and mortality rates and causes consequent final damage to organ.7 Total energy requirements in the infant and children who are comprised of energy are increased to maintain metabolism and energy required for growth. The child with CHD contents with potential hypermetabolism, decreased mesenteric perfusion, difficulty in feeding. Providing optimal nutrition in this population can improve surgical outcomes. Children with pulmonary hypertension are prone to growth retardation and malnutrition.8 To prevent the morbidity and mortality associated with malnutrition in children with CHD, an aggressive evidence-based management must be enacted. Proper nutritional management provides a good opportunity to significantly affect these parameters.8 While some children improve on nutritional counselling there are some who cannot have large amount of high energy feeds hence need a different approach.9 One study by Jeffrey et al has shown that percutaneous endoscopic gastrostomy (PEG) is a safe feeding technique to provide more calories to those children who are severely malnourished due to CHD. 1 This method of feeding has an advantage that the child will not utilize any extra energy to feed and therefore more stores are available for growth. In a study done in Egypt by Hassan et al.7 total prevalence of malnutrition was 84% in patients. Severe malnutrition was seen in 71.4% of cases. In patients with acynotic CHD, stunting was significantly higher (57.89%), while wasting was more (45.83%) in cyanotic CHD7. Children with congenital heart diseases (CHD) are observed to have poor nutritional status.10 Malnutrition is a big issue amongst children in developing countries due to poor socioeconomic issues, ignorance and increased incidence of preventable infectious diseases. Thus, children with CHD from resource poor countries are at higher risk of severe malnutrition due to their exposure to above factors.11 “Study conducted on malnutrition among under five children in Bangladesh revealed that household socioeconomic status, mother’s antenatal visit (s), and mother’s BMI are the most important determinant s of child’s malnutrition.12 In a study done in Nigeria low maternal income and overcrowding were associated with higher occurrence of wasting and no association was found between the source of drinking water or social class and malnutrition”.13 “The severity of malnutrition can range from mild undernutrition to failure to thrive. This has a notable effect on the outcome of surgery, increase in morbidity and mortality. Different types of cardiac defects can affect nutrition and growth in different stages”14 Most treatment strategies aim to provide extra calories and protein that exceed the Recommended Dietary Allowance for age thereby promoting catch up growth. However, there is no generally accepted set of guidelines that define appropriate caloric intake for catch-up growt.15 “A study done in Nigeria done on children with CHD were of the view that the most important potent trigger of severe malnutrition among children with congenital heart disease is pulmonary hypertension.16 Similar findings were seen in the study by Pitmann et al, they also noted the impact of pulmonary hypertension on growth and nutrition in cyanotic and acyanotic heart disease, and found that cyanotic patients with pulmonary hypertension were more affected than acyanotic children with pulmonary hypertension.17 Another factor that causes malnutrition among children with congenital heart disease in this study was dietary inadequacy. This has a negative effect on nutrition and growth of children with CHD.16 Progressive decline in nutritional status is associated with active and poorly controlled disease, deteriorating cardiac function and morbidity and mortality.
Aim & Objectives
To assess the nutritional status in patients with CHD using clinical evaluation, anthropometry, to know the effect of different types of congenital heart diseases on growth, to correlate the severity of malnutrition with the type of lesion or specific lesion.
Materials and Methods
It is a cross-sectional observational stud. In our study a total of 75 cases of congenital heart disease were examined in a period of 18 months. Only those children will be enrolled in the study whose parents / guardians agree to the informed consent. The decision of consultant (guide) will be final while considering inclusion of cases.
Inclusion criteria
All children with CHD attending paediatric cardiology outpatient department. All children with CHD admitted in hospital for LRTI or any other sequelae of CHD/malnutrition who are stable.
Exclusion criteria
Those who have undergone corrective interventions either catheter or surgically palliated or corrected CHD. Those with secondary malnutrition due to HIV, TB and chronic illnesses other than CHD. Any serious acute illnesses requiring ICU admission.
Methodology
Those who fulfil the eligibility criteria will be enrolled after explaining nature of the study to the parents and obtaining a written informed consent. Signs and symptoms of heart disease (as per NADAS criteria) will be screened after thorough clinical evaluation and also by 2D ECHO. {NADAS criteria: A) major criteria- systolic murmur grade 3 or more, diastolic murmur, cyanosis, CHF; B) minor criteria – systolic murmur <grade 3, abnormal second heart sound, abnormal ECG, abnormal CXR, abnormal BP FOR DIAGNOSIS OF CHD- 2MAJOR OR 1 MAJOR + 2 MINOR} Anthropometric measurements including weight(kg), height/length(cm), head circumference(cm), MUAC (cm), chest circumference(cm), BMI and weight/height will be performed as per WHO procedures. Z scores for weight for age (WAZ), weight for height (WHZ), height for age (HAZ) will be calculated. After calculation of WAZ, HAZ, WHZ the studied groups will be classified into normal nutrition or moderate malnutrition (WHO) or severe acute malnutrition (SAM). < -2sd to <-3sd WAZ OR HAZ OR WHZ will be classified respectively as underweight or stunted or wasted and <-3sd WAZ OR HAZ will be classified respectively as severely underweight or severely stunted or severely wasted. From these classified individuals, patterns of malnutrition will be assessed in specific type of lesions with and inference will be made on which groups are predominantly stunted and which are wasted. Further its effect on the disease course will be seen by considering multiple factors like how many times a particular class for example cyanotic group has been hospitalized or has had refractory CHF, number of times acynotic CHD cases developed respiratory tract infections and so on. Nutritional counselling will be done as per WHO guidelines and dietician advise.
Results
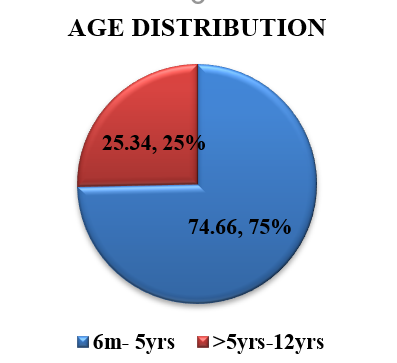
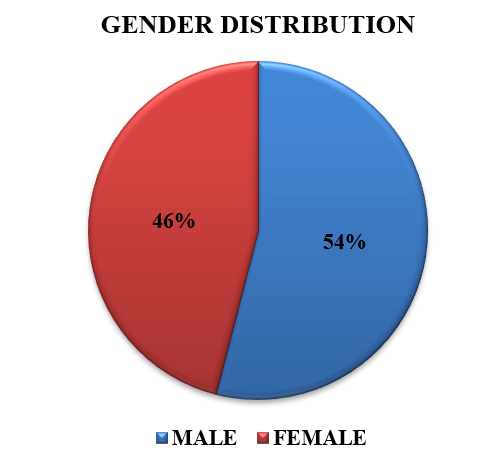
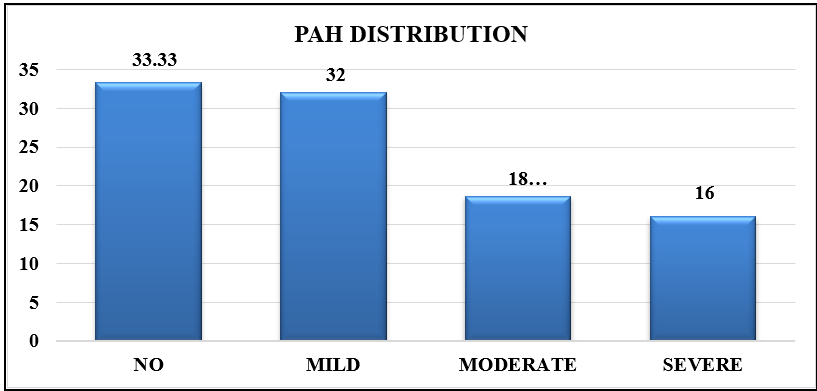
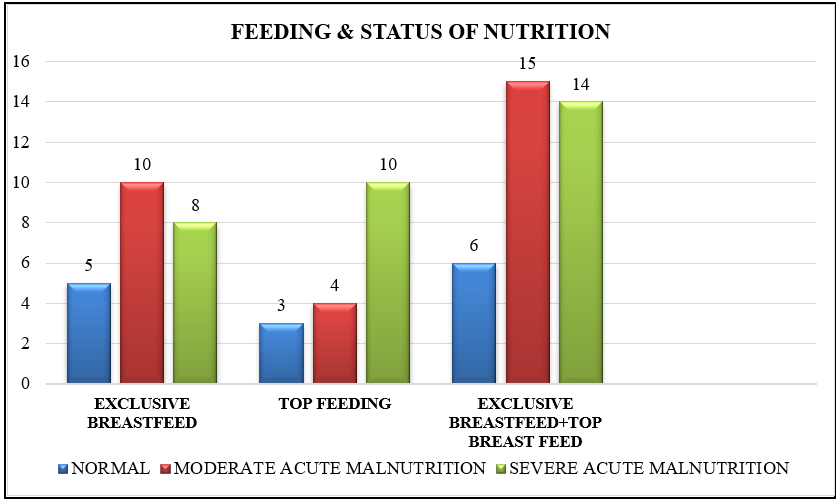
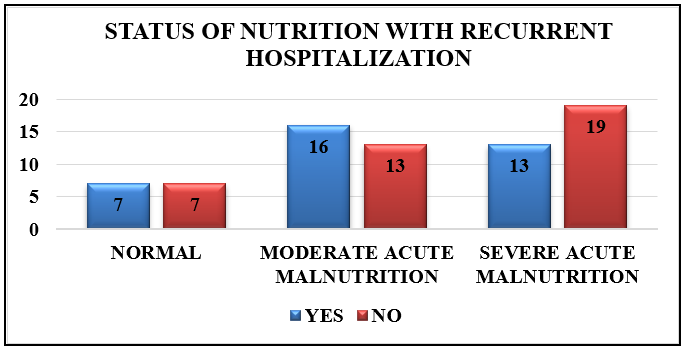
Out of 75 patients 56 (74.66%) were <=5years and 19(25.34%) were >5years to 12 years. 40 (53.3%) males and 35 (46.67%) females were having CHD. Out of 75 patients with congenital heart disease 47 (62.66%) were having acyanotic heart disease and 28 (37.33%) were having cyanotic heart disease. Out of 75 cases and out of 47 (62.66%) acyanotic heart disease children 24(32%) had Ventricular Septal Defect as the most common lesion; out of 28 cases of cyanotic heart disease 20(26.66%) had TOF as the predominant lesion. A correlation was observed between recurrent LRI with the types of CHD; and it was found that recurrent LRI is predominant with acyanotic heart disease though there is no significant association statistically. Out of 75 cases 47 were acyanotic out of which 26(55.3%) cases showed history of recurrent lower respiratory tract infection while out of 28 cyanotic heart disease cases only 10(35.71%) showed history of recurrent lower respiratory tract infection. In present study malnutrition was predominantly observed in middle class, though it was statistically not significant. In present study malnutrition was predominantly observed in middle class, though it was statistically not significant. According to this study malnutrition was predominantly (85.1%) seen in acyanotic heart disease. Thus, stunting was more observed in cyanotic heart disease. Underweight was more observed in acyantoic heart disease which is statistically significant.
Table 1
Type of CHD and the most common specific lesion amongst CHD cases
|
Type of CHD |
No. of Patients |
Percentage (%) |
|
|
Acyanotic |
VSD |
24 |
32 |
|
ASD |
10 |
13.33 |
|
|
PDA |
11 |
14.66 |
|
|
Cyanotic |
TGA |
02 |
2.67 |
|
TAPVC |
03 |
4 |
|
|
TOF |
20 |
26.66 |
|
|
DORV |
03 |
4 |
|
Table 2
Association between types ofchd & recurrent LRI
|
Type of CHD |
Recurrent LRI |
Total |
Chi-square value |
p-value |
|
|
Yes |
NO |
||||
|
Acyanotic |
26 |
21 |
47 |
2.702 |
0.100 |
|
Cyanotic |
10 |
18 |
28 |
||
|
Total |
36 |
39 |
75 |
||
Table 3
Association between socioeconomic status and nutritional status
Table 4
Anthropometry measurement
Table 5
Association between types ofchd & status of nutrition
Table 6
Association between types of PAH & status of nutrition
|
PAH |
Status of nutrition |
Total |
|
|
Normal Nutrition |
Malnutrition (MAM+SAM) |
||
|
No PAH |
06 |
19 |
25 |
|
Mild |
04 |
20 |
24 |
|
Moderate |
03 |
11 |
14 |
|
Sever |
01 |
11 |
12 |
|
Total |
14 |
61 |
75 |
Table 7
Association between types of CHD & status of wasting, stunting and underweight
Discussion
Out of 75 patients with congenital heart disease 47 (62.66%) were having acyanotic heart disease and 28 (37.33%) were having cyanotic heart disease. Our study findings were similar to a number of studies, like in a study by Hassan et al 7 published in 2015 on ‘Nutritional Status in children with un-operated congenital heart disease: an Egyptian center experience’ they reported that maximum children in their study suffered from acyanotic CHD 76/100 (76%). Ratanachu-ek et al 18 in their study ‘Nutritional Status of Pediatric Patients with Congenital Heart Disease: Pre and Post Cardiac Surgery’ published in 2011 reported maximum cases of acyanotic heart disease (79.5%) quite similar to this study. Okoromah et al 19 in their study ‘Prevalence, profile and predictors of malnutrition in children with congenital heart defects: a case control observational study’ published in 2011 reported acyanotic heart disease in 48/73 cases (65.75%) quite similar to our study. In a study by Iseuzuo et al 20 ‘Nutritional Status of children with congenital heart diseases at a University Teaching Hospital, North Western Nigeria’ published in 2017 they reported predominantly acyanotic heart disease in 62/90 cases (68.88%). In a study done in India by Bhardwaj et al 21‘Epidemiology of Congenital Heart Disease in India’ published in 2015, 66% cases were reported to have acyanotic heart disease similar to our study. So, this gives a broad estimate of incidence and prevalence of acyanotic heart disease being higher in most children with CHD compared to those with cyanotic heart disease. In a study done by Khalil et al 22 ‘Incidence of Congenital Heart Disease Among Hospital Live Births in India’ published in 1993 they found a high prevalence of cases with Ventricular Septal Defects in 34.8% of all cases diagnosed as CHD. In a study by Iseuzuo et al 20‘Nutritional Status of children with Congenital heart Diseases at a University Teaching Hospital, North Western Nigeria’ published in 2017 they reported most common heart disease as Ventricular Septal Defect seen 42.2% cases similar to our study. A study done by Varan et al[23 on ‘Malnutrition and growth failure in cyanotic and acyanotic congenital Heart disease with and without pulmonary hypertension” published in 1998 documented that 26/89 (29.21%) cases of CHD had pulmonary hypertension all suffering from acyanotic heart disease, while 16/89 (19.79%) cases with cyanotic heart disease were having pulmonary hypertension. Unlike this study most of the studies show a higher prevalence of pulmonary hypertension like in a study done by Bedford et al[24] ‘Atrial Septal Defect and Its Surgical Treatment’ published in 1957 he found only 15% of cases with ASD with obstructive PAH not similar to findings we have. In the study done by Hassan et al 7, ‘Nutritional Status in children with un-operated congenital heart disease: an Egyptian center experience’ published in 2015 where the overall prevalence of moderate acute malnutrition was 60% in patients with congenital heart disease and severe acute malnutrition was diagnosed in 24% cases. Okoromah et al 19 in their study ‘Prevalence, profile and predictors of malnutrition in children with congenital heart defects: a case control observational study’ published in 2011 reported severe acute malnutrition was 61.6% and moderate acute malnutrition was found in 28.76% cases. Okoromah et al 19 in their study ‘Prevalence, profile and predictors of malnutrition in children with congenital heart defects: a case control observational study’ published in 2011 reported 20.5% cases had underweight, 21% cases had stunting, 30% cases had wasting. Hanan m. abdelmoneim et al 23, ‘Assessment of Nutrition State in Children with Heart Diseases’ published in 2019 reported that 11.6% cases had underweight, 27.9%cases had stunting,60.4% cases had wasting. In a study by Okoromah et al 19 on ‘‘Prevalence, profile and predictors of malnutrition in children with congenital heart defects: a case control observational study’ published in 2011 they found that wasting was predominant in acyanotic heart disease seen in 28/48 (58.37%) acyanotic CHD cases, which is similar to this study where wasting was seen in 40/47 (90.9%) acyanotic CHD cases but here wasting was also seen in 21/28(75%) cyanotic CHD cases thus making it statistically non-significant; and stunting was seen in 17/25(68%) cyanotic heart disease, which is also similar to this study where stunting was seen in 18/28 (64%) cyanotic CHD cases. In a study by Schwarz et al 24 on ‘Enteral Nutrition in Infants with Congenital Heart Disease and Growth Failure’ published in 1990 in which they noticed that on serial anthropometric measurements demonstrated that only 24-hour infusions of nasogastric feeds were associated with significantly improved nutritional status, when assessed by z scores for weight (P <0.01) and length (P < .05). Group 1 infants also showed marked increases in midarm muscle circumference and triceps and subscapular skinfold thicknesses (P < .01, compared with other 2 groups receiving 12hr feeds or oral feeds’ hence proving our finding that some other method of feeding should be practiced.
Conclusion
This study thus concludes that maximum children with congenital heart disease have malnutrition, more commonly seen in those with acyanotic heart disease and maximum children present with wasting hence classified under those having severe acute malnutrition. that there are multiple factors that are responsible for malnutrition in children with CHD including, poor socioeconomic strata, already poor health conditions in the general population, recurrent hospitalizations and recurrent lower respiratory tract infections. A different approach to the feeding strategies is needed and a general consensus regarding which method of feeding to use and what to feed the child should be met in our country. The above-mentioned factors have an adverse effect on the progression of disease and vice versa but we don’t get a proper idea on the prognosis of these cases based on these risk factors. More studies should be done in our country to find out counteractive measures to reduce the prevalence of malnutrition in these children and to see the effect of pre-operative nutrition on post cardiac surgery in children.