Introduction
Heart failure a chronic progressive condition, significantly impacts patients' quality of life by impairing their cardiac function, leading to reduced blood flow and oxygen to the body's organs and tissues.1 The complexity of heart failure lies in its multifaceted nature, affecting not only the physical but also the psychological and social aspects of individuals' lives. Among the myriad challenges faced by patients with heart failure, the quality of sleep and their ability to perform activities of daily living (ADL) are critical yet often overlooked dimensions.2 This study aims to delve into these aspects, providing insights into the interplay between heart failure, sleep quality, and ADL. The significance of understanding these relationships lies in the potential to improve management strategies and patient outcomes.
Heart failure remains a leading cause of hospitalization and morbidity worldwide, with an estimated prevalence that continues to rise due to the ageing population and the increasing prevalence of predisposing factors such as hypertension, diabetes, and coronary artery disease.3 The condition is characterized by the heart's inability to pump sufficient blood to meet the body's needs, leading to symptoms like breathlessness, fatigue, and fluid retention, which severely limit physical activities and impact patients' quality of life. 4
Sleep disturbances, including insomnia, sleep-disordered breathing, and nocturnal dyspnea, are common among patients with heart failure, affecting up to 75% of the population.5 These disturbances are not merely symptoms of the condition but contribute to its progression through mechanisms such as increased sympathetic nervous system activity and elevated proinflammatory cytokine.6 Recent research has highlighted the reciprocal relationship between sleep quality and heart failure, suggesting that poor sleep may exacerbate heart failure symptoms, while improved cardiac function can lead to better sleep outcomes. 7
Activities of daily living (ADL), encompassing basic tasks necessary for personal care, are significantly affected in patients with heart failure. The reduced physical capacity resulting from heart failure compromises the ability to perform ADL independently, affecting bathing, dressing, eating, and even ambulation.8 The impairment in ADL is a critical determinant of the quality of life and is associated with higher rates of hospitalization and mortality among CCF patients. 9
The relationship between sleep quality and ADL in heart failure patients is complex and bidirectional. Poor sleep quality can lead to daytime fatigue, reduced physical activity, and diminished motivation, further impairing ADL performance.10 Conversely, limitations in performing ADL can lead to increased stress and anxiety, which in turn may disrupt sleep patterns. Understanding this interplay is crucial for developing comprehensive care plans for heart failure patients.
A research study by Ghane et al. (2022) investigated the impact of a tailored sleep intervention on the sleep quality and daily functioning of patients with heart failure, demonstrating significant improvements in both sleep quality and ADL performance among those who received the intervention, compared to the control group. 11 These findings underscore the potential benefits of integrating sleep management strategies into the care of heart failure patients. Another study by J Lin et al. (2023) explored the associations between demographic factors, sleep quality, and ADL in a cohort of heart failure patients. The researchers found significant correlations between poor sleep quality and impaired ADL, with age, gender, and comorbid conditions as key influencing factors.12
Materials and Methods
This study employed a quantitative, non-experimental research, cross-sectional, design, focusing on evaluating sleep quality among elderly patients at the cardiology outpatient department in a teaching hospital in South India. The study was conducted after the formal permission from the concerned department. Over four weeks, the research aimed to provide a snapshot of sleep quality and activity of daily living. A total of 50 individuals were selected through a non-probability, convenience sampling method. This technique was chosen to align with the study’s objectives, allowing for the selection of participants based on their availability and willingness to participate without the need for random sampling.
The inclusion criteria for participant selection were well-defined, encompassing patients who can understand English or Tamil, are aged 20 and above, both male and female and are willing to participate. Exclusions were made for individuals with mental challenges or those experiencing severe pain during their outpatient department visits. The research tools utilized, aimed at assessing Activities of Daily Living (ADL) and the Pittsburgh Sleep Quality Index (PSQI) scores among patients with congestive cardiac failure, were validated through content validity by experts in the Nursing and Medical fields. These tools demonstrated high reliability, evidenced by Cronbach's alpha scores of 0.87 for ADL and 0.80 for PSQI, indicating their effectiveness in meeting the study’s goals.
The questionnaire was divided into two sections: the first part gathered socio-demographic information such as age, sex, education, and other relevant details, while the second part evaluated sleep quality using the PSQI and ADL through a checklist. The PSQI assessed various aspects of sleep quality, including subjective sleep quality, sleep latency, and disturbances, among others. The scoring was designed to identify levels of independence or the need for assistance in the participants. The analysis plan of the study was structured to employ descriptive and inferential statistics, with demographic data analyzed through frequency and percentage distributions and sleep quality scales assessed using mean, median, mode, and standard deviation.
Results
The study aimed to evaluate the sleep quality and Activities of Daily Living (ADL) and the association between patient’s selected demographic variables with levels of ADL and PSQI scores among the participants. The demographic distribution indicated a higher percentage of participants aged between 51-60 years (52.00%), with an equal distribution between male and female participants (50.00% each). The majority were self-employed (50.00%) and had a primary level of education (46.00%). The income distribution showed a substantial portion of participants earning between Rs. 10001-29972 (50.00%). The type of family most participants belonged to was nuclear (52.00%), with a significant number not engaging in exercise (74.00%) and following a non-vegetarian diet (66.00%).
Activities of living score
The Table 1 represents the Activities of Living Score, comprising 14 activities each with a maximum score of 3. The mean scores range from 1.46 to 2.10, reflecting a variation in the degree of independence in performing these activities. The overall average percentage of the mean score across all activities is 57.05%. Activities like dressing and bathing scored higher (70% and 68% respectively), while climbing stairs and walking are among the lowest (48.67% and 51.33% respectively), indicating varied functional capabilities among individuals.
Table 1
Percentage of activities of living score
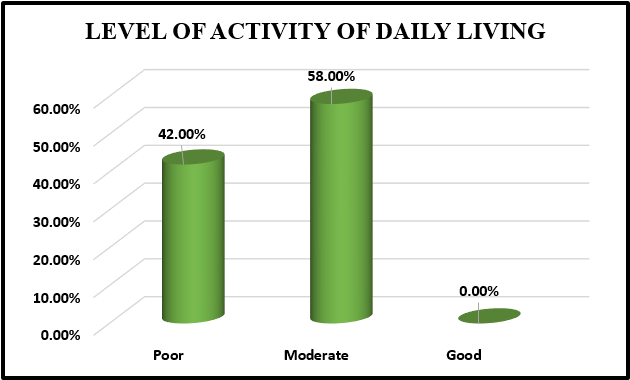
Level of activity of daily living
Data revealed that a significant portion, 42%, are classified with poor ADL scores, while 58% fall under moderate. Notably, none of the patients were assessed with a good level of ADL score. (Figure 1)
Level of sleep quality
Outlines the component-wise Sleep Quality Score, capturing seven components, each evaluated by a mean score and standard deviation (SD). Notable findings include higher sleep disturbances (mean=1.56) and sleep latency (mean=1.44), with the use of sleeping medications being the lowest (mean=0.77). The total Global Pittsburgh Sleep Quality Index (PSQI) score aggregates to 8.11, with a standard deviation of 4.55, indicating variability in sleep quality among respondents.
Table 2
Component wise sleep quality score
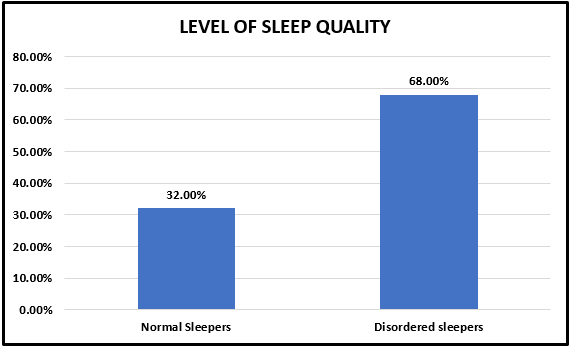
Level of sleep quality
The data categorizes 50 individuals into normal and disordered sleepers based on their sleep scores. A significant majority, 68%, are identified as disordered sleepers, while only 32% fall into the normal sleepers category. This distribution underscores a prevalent issue of sleep disorders among the studied group. (Figure 2)
Association Between ADL and sleep quality with Demographic Variables
A significant association was observed between age and ADL score (χ2=11.53, P=0.01), particularly notable in the 61-70 years age group, which showed a majority (73.33%) having poor ADL scores. No significant associations were found with gender, education, occupation, monthly income, type of family, exercise, diet pattern, BMI, or personal habits, suggesting that these factors do not significantly influence ADL scores within this population.
Similar to the ADL score associations, a significant correlation was observed between age and PSQI score (χ2=11.52, P=0.01), with older participants more likely to have disturbed sleep patterns. The rest of the demographic variables did not show a significant association with PSQI scores, indicating that factors such as gender, education, occupation, income levels, and lifestyle habits may not directly impact sleep quality in this study group.
The results of this study highlight the impact of age on both ADL and PSQI scores, suggesting that older adults are more susceptible to lower ADL scores and disturbed sleep patterns. These findings emphasize the need for targeted interventions to improve the quality of life and sleep among older populations.
Discussion
In this study, the examination of Activities of Living (ADL) and sleep quality among heart failure patients revealed nuanced insights into their daily challenges and sleep patterns. A notable observation was the variation in ADL scores, with dressing receiving the highest percentage score of 70%, indicating a relatively better capacity among patients to manage dressing themselves. In contrast, climbing stairs emerged as the most challenging activity, with the lowest score of 48.67%. This disparity in ADL capabilities underscores the range of physical limitations faced by these patients, reflecting the impact of their cardiac conditions on daily functions. The ADL scores further categorized patients into two main groups: 42% with poor ADL scores and 58% with moderate scores, assessed via a checklist. This classification highlights the predominance of moderate functional impairment in this patient cohort, suggesting a significant need for targeted support and interventions to enhance their daily living capabilities. This was supported by a study conducted by Roy et al. (2022) which showed that 73.9% reported difficulty with activities of daily living at diagnosis.13
Sleep quality, a critical aspect of overall well-being, was also scrutinized, revealing that 32% of the participants had normal sleep scores, while a striking 68% experienced disordered sleep. This was supported by a study conducted by Getahun et al. (2022) which showed that majority of the cardiac patients 62.2% were considered to have poor sleep status while the remaining 37.8% were considered as good sleepers.14
The examination of demographic variables revealed significant associations with both ADL and PSQI scores. Age was a critical factor, showing a strong association with both ADL and sleep quality scores, emphasizing the heightened vulnerability of older patients to both functional limitations and sleep disturbances. However, other demographic factors such as sex, occupation, and monthly income showed less consistent associations, indicating that while demographic characteristics can influence ADL and sleep quality, they do so in complex and varied ways. The study's findings advocate for comprehensive patient support systems that not only address the physical manifestations of cardiac conditions but also consider the broader implications on patients' daily lives and sleep health. This was supported by a study conducted by Esnaasharieh et al. (2022) which showed a strong association between age of the patients with sleep quality and activity of daily living. 15
Conclusion
This study showed the significant impact of heart failure (HF) on patients' sleep quality and activities of daily living (ADL), with a substantial proportion experiencing disordered sleep and diminished ability to perform daily tasks. These findings underscore the necessity of integrating comprehensive care strategies that encompass not only medical treatments but also lifestyle modifications, sleep management, and support for daily activities. Such an approach could greatly enhance the quality of life for heart failure patients. Future research should delve into the efficacy of multidisciplinary interventions aimed at improving both sleep quality and ADL in this vulnerable population.