- Visibility 84 Views
- Downloads 2 Downloads
- DOI 10.18231/j.ijpns.2022.007
-
CrossMark
- Citation
Clinical case report on bipolar affective disorder, mania
- Author Details:
-
Javaid Ahmad Mir *
-
Bushra Mushtaq
-
Onaisa Aalia Mushtaq
Introduction
Diagnose: Bipolar effective disorder (BPAD) currently in mania
Chief complaints: X years old male patient, Mr. ABC, unmarried living in nuclear family belonging to lower middle class of low socioeconomic status, residing at XXXXXXXXX, presented with complain of:
Irritability-2 months.
Increased psycho motor activity (PMA)- 10 days.
Hyper religious behavior-2 months.
Suspiciousness-1 year.
Decreased sleep and decreased appetite.
Precipitating factor: Substance abuse.Predisposing factor: Family history of psychiatric illness.Perpetuating factor: Continuous substance abuse.
History of present illness
Patient was in his usual state of health 1 year back when he started with suspiciousness in the form of suspecting that people are going to harm him. However, no amount of reassurance was able to help him or convince him otherwise. He started to demand Rs.15 lac from his father saying that he should return him the money that he has earned during the past 5-6 years. He would say that he will settle down in Jammu with his Muslim brothers. Finally, his parents gave him a rented accommodation at Srinagar in October 2013. His mother stayed with him for about 2 months during which the patient did not do any productive work. After this his mother left for Jammu. About three months later the patient’s neighbor called his parents and told that their son has decreased self-care and substance abuse and that they should came. His mother then came and observed that the patient would get easily annoyed over minor issues and start shouting whenever she tried to counsel him, he would either get aggressive or go out of home. The patient would at times become mute altogether for 2-3 hours. The patient also had hyper religious behavior in the form of offering Namaz and Tajhud and spending most of his day in praying. The patient also had restlessness and would leave his home early in the morning then walk about 2-3 kms. And return home. The patient would also have decreased sleep and never complain about it. The patient also had decreased intake of food and it progressed to total refusal of food.History of past illness: Not significant.
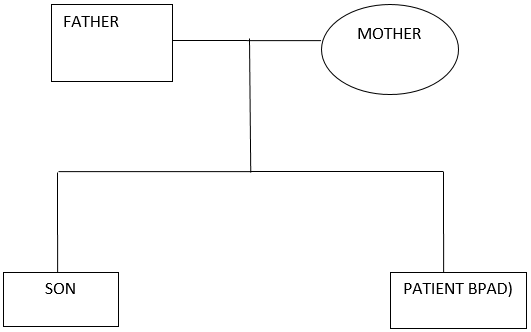
Family tree
Substance abuse history: Cannabis abuse for the past 6 years, Abstinence for the past 2 months.Forensic history: Nil.
Personal history
Birth and early development: FTND (Full term normal delivery), no history suggestive of any antenatal, natal and postnatal complications.
Presence of childhood disorder: Nil
Home atmosphere in childhood and adolescence: Lived in joint family and used to often fight with elders over property issues.
Scholastic and extracurricular activities: Studied up to class 7th then left studies did not appear in class 8th exams. He changed multiple schools.
Vocation: Worked as auto driver, shopkeeper (for 1 year) and did government job for a period of 6 months and after that changed work multiple times and would never give any sufficient reason for changing job.
Marital history: Unmarried.
Premorbid personality
Seff: Predominant mood cheerful and made many friends.
Relations: Preferred Company of many friends.
Did Not have very high religious standards (Offers Nimaz) occasionally but took good care of:
Drugs prescribed for the patient
Tab valproic acid 500 mg BD.
Inj. olanzapine 10 mg OD.
|
Name of Drug |
Mechanism of Action |
Dosage/ Route |
Indication |
Contrain- DictionI |
Side Efects |
Nurse S Role |
|
Valproic acid (depakene, depakote) |
Action in the treatment of bipolar disorder is unclear. |
500 mg/oral |
Epilepsy, manic episodes, migraine prophylaxis and adjunct therapy in schizophrenia. |
Hypersensitivity, liver disease, cardiac disease, pregnancy and lactation. |
Blood dyscriasis Prolonged bleeding time. |
Ensure that the client understands the importance of regular blood tests while receiving anticonvulsant therapy. Ensure that platelet counts and bleeding time are determined before initiation of therapy with valproic acid. Monitor for spontaneous bleeding or bruising. |
|
Inj olanzapine (zyprexa) |
Action in the treatment of mania is unclear |
10-20 mg/ iv |
Schizophrenia,acute manic episodes, agitation associated with mania or schizophrenia |
Hyppersensitivity, children, lactation. hepatic, cardiovascular disease, history of seizures narrow angle glaucoma diabetes pregnancy |
Drowsiness, dizziness, Dry mouth, Weight gain, ECG changes, hyperglycemia |
1. Ensure that the client does not operate dangerous machinery or participate in activities that require alertness. 2. Provide sugarless cansdyor gum or ice and frequent sips of water. 3. Provide calorie controlled diet. 4. Monitor vital signs. Observe for symptoms of dizziness, syncope or weakness. 5. Monitor blood glucose regularly. |
|
Presentation |
Key features |
|
Mania |
Elevated, expansive or irritable mood With or without psychotic symptoms Marked impairment in functioning. |
|
Hypomania |
Elevated, expansive or irritable mood No psychotic symptoms Less impairment of functioning. |
|
Depression |
Mild, moderate or severe With or without psychotic symptoms. |
|
Rapid cycling |
At least four episodes in 1 year. |
|
Mixed states |
Manic and depressive features present during same episode. |
Description of disease
Definition of bipolar disorders
Bipolar disorder is an episodic, potentially life-long, disabling disorder that can be difficult to diagnose. Need to improve recognition, reduce sub-optimal care and improve long-term outcomes. There is variation in management of care across healthcare settings.[1]
Characteristics of a manic episode
A Distinct period of abnormally and persistently elevated, expansive or irritable mood.
During the period of mood disturbance, at least three of the following symptoms have persisted (four if the mood is only irritable) and have been persistent to a significant degree[2] a) Inflated self-esteem or grandiosity, b) Decreased need for sleep, c) More talkative than usual or pressure to keep talking d) Flight of ideas or subjective experience that thoughts are racing e) Distractability, i.e. attention too easily drawn to unimportant or irrelevant external stimuli, f) Increase in goal-directed activity or psychomotor agitation g) Excessive involvement in pleasurable activities which have a high potential for painful consequences, e.g. unrestrained buying sprees, sexual indiscretions, or foolish business investments.
Mood disturbance sufficiently severe to cause marked impairment in occupational functioning or in usual social activities or relations with others, or to necessitate hospitalization to prevent harm to self or others.
At no time during the disturbance have there been delusions or hallucinations for as long as two weeks in the absence of prominent mood symptoms.
Not superimposed on schizophrenia, schizophrenic form disorder, or delusional disorder or psychotic disorder
The disturbance is not due to the physiologic effects of a substance or general medical disorder
|
C linical manifestations according to Book |
C linical manifestations in Patient |
|
1. Elevated expansive or irritable mood 2. Inflated self-esteem or grandiosity 3. Decreased need for sleep 4. More talkative than usual 5. Flight of ideas or subjective experience that thoughts are racing 6. Distractibility 7. Increase in goal directed activity (either socially, at work or school or sexually) or psychomotor agitation 8. Excessive involvement in pleasurable activities that have a high potential for painful consequences. |
Euphoria Irritability Increased psychomotor acivity Hyperreligious behavior Decreased sleep and appetite Suspiciousness |
|
D iagnosis according to Book |
D iagnosis done in Patient |
|
History taking Mental Statue Examination(MSE) Physical examination[3] |
History taking MSE Physical examination blood tests |
|
Management according to Book |
Management done in Patient |
|
1. Individual psychotherapy 2. Group psychotherapy 3. Family therapy 4. Cognitive therapy 5. Electroconvulsive therapy 6. Psychopharmacology Antimanic (lithium carbonate-1800-2400mg) Anticonvulsants I:e, carbamazepine (tegretol-200-1600mg) clonazepam(klonopin-0.5-20mg) Valproic acid(depakote-5mg/kg to 60mg/kg Lamotrigine (lamictal-100-200mg) Gabapentin (neurontin-900-1800mg)[4] Calcium channel blockers I:e,verapamil-80-320mg Antipsychotics I:e, olanzapine Chlorpromazine Quetapine Risperidone Ziprasidone |
1. Individual psychotherapy 2. Group psychotherapy 3. Cognitive therapy Valproic acid i:e, 500mg Olanzapine i:e, 10 mg |
|
Sr. No. |
Lab Test |
Patient Value |
Normal Value |
Remarks |
|
1. |
CBC: Haemoglobin TLC MCV HCT WBC LYMPH NEUT MONO EISONO BASO PLT |
10gm/dl 6.03/cumm 81.3fl 40% 12.32 18.4% 68.9% 6.8% 5.7% 0.2% 258/cumm |
13-18gm/dl 4,500-11000/cumm 75-95fl 40-50% 4-10/cumm 20-25% 40-75% 01-10% 1-6% 00-01% 140-440/cumm |
Decreased Normal Normal Normal Increased Decreased Normal Normal Normal Normal Normal |
|
2. |
KFT: Urea Creatinine |
42mg/dl 0.6mg/dl |
10-50mg/dl 0.5-1.5mg/dl |
Normal Normal |
|
3. |
ELECTROLYTES: Na+ K+ |
138mmol/L 3.6mm0l/L |
135-145mmol/L 3.5-5.0mm0l/L |
Normal Normal |
|
4. |
SERUM CHEMISTRY: Uric acid Calcium Blood glucose; Fasting Post prandial |
6.0mg/dl 6.1mg/dl 93mg/dl 130mg/dl |
2.5-8mg/dl 8.6-10.2mg/dl 60-110mg/dl 65-140mg/dl |
Normal Normal Normal Normal |
|
5. |
LFT: Bilirubin AST ALT ALP Albumin |
1.03mg/dl 22U/L 16 U/ml 55UL 3.09g/dl |
0.3-1.0mg/dl 15-30U/L 8-35U/ml 50-120UL 3.5-5.5g/dl |
Normal Normal Normal Normal Normal |
|
Date |
Time |
Temp |
Pulse |
Respiration |
Blood Pressure |
Summary |
|
7/6/14 |
10:30AM |
98.7OF |
78/MIN |
20/min |
130/90mmHg |
Patient is conscious, oriented to time, person and place. Mood: “theek” but affect slightly elevated Speech: Increased tone and volume Perception: Has persecutory delusions, and auditory, hallucinations Psychomotor activity(PMA): Increased Insight: Grade 1st PT’S vitals were checked, prescribed medicines were administered. |
|
8/6/14 |
10:00am |
98.60f |
64/min |
16/min |
120/80mmHg |
Pt was conscious, oriented to time, place and person, sitting on bed, well groomed Mood: “bilkul theek” affect happy and congruent Speech: Non spontaneous increased tone and volume Perception: has persecutory delusions, Psychomotor activity(PMA): Increased Insight: Grade 1st PT’S vitals were checked, prescribed medicines were administered and blood tests were done |
|
9/6/14 |
10:00am |
98.60f |
78/min |
24/min |
110/70mmHg |
Pt looks conscious but oriented to time, place and person. Elderly tall, lean but well-dressed adequately groomed and eye contact established. Mood: “theek ” affect sad Speech: normal tone, rate and volume Perception: Has persecutory delusions. Psychomotor activity(PMA): Normal Insight: Grade 1st Pts general condition seems satisfactory, vitals checked. |
|
10/6/14 |
10:30am |
98of |
74/min |
24/min |
120/90mmHg |
Pt looks drowsy but oriented to time, place and person Mood: “Asal” affect incongruent Speech: decreased tone, rate and volume Perception: has persecutory delusions Psychomotor activity(PMA): Decreased Insight: Grade 2nd Vitals checked. Prescribed medicines were given, patient told that he wants to go to home. |
|
11/6/14 |
11:00am |
980f |
72/min |
20/min |
120/80mmHg |
Pt was conscious, oriented to time, place and person, medicenes were admininisterd, specific blood tests were done. Mood: “khush” affect inapprppriate Speech: Normal tone, rate and volume Perception: Denies any hallucination Psychomotor activity(PMA): Normal Insight: Grade 1st |
|
Nursing Diagnosis |
Outcome Criteria/OBJ. |
Intervention |
Rationale |
Evaluation |
|
1. Risk for injury related to manic episode evidenced by extreme hyperactivity, increased agitation and lack of control. |
Short Term Goal: Within a specified time client will be able to recognize signs of increased agitation and hyperactivity. Long Term Goal: Client will be able to to have control over injurious movements and will not harm himself. |
1. Reduce stimuli. 2. Assign private room. 3. Remove hazardous objects from area like scissor, knife. 4. Stay with the client when he is agitated. 5. ranquilizers as ordered. |
1. To prevent injury. 2. For close observation of patient. 3. To prevent self-injury. 4. It gives him a feeling of security. 5. If hyperactivity increases. |
No longer experiencing physical symptoms. |
|
2. Risk for violence self-directed or other directed related to increased psychomotor activity evidenced by manic excitement, delusional thinking. |
Short Term Goal: Within a specified time client will recognize signs of increased anxiety and agitation and report to staff for assistance with intervention. Long Term Goal: Client will not harm self or others. |
1. Maintain alow level of stimuli in the client’s environment. 2. Observe the client’s behavior frequently. 3. Remove all dangerous objects from the client’s environment. 4. Maintain a calm attitude Towards a patient. 5. Offer some alternatives in a physical activity (e:g, punching bag, physical exercise). |
1. Anxiety level rises in a stimulating environment. 2. Close observation is necessary so that intervention can occur if required to ensure client’s safety. 3. So that in his or her agitated state the client may not use them to harm self or others. 4. As the client’s anxiety decreases. 5. It gives him a feeling of some control over the situation. |
Client has not harmed self or others. Client verbalizes which of his Interaction behaviours are appropriate and which are inappropriate. Eats a well-balanced diet. Nutritional status restored. Client sleeps 4-6 hrs without awakening. |
|
3. Impaired social interaction related to delusional thought process (delusion of persecution) underdeveloped ego and low self-esteem. Evidenced by inability to develop satisfying relationships. |
Short Term Goal: Client will verbalise which of his interaction behaviours are appropriate and which are inappropriate within 1 week. Long Term Goal: Client will demonstrate use of appropriate interaction skills. |
1. Recognise the purpose these behaviours serve for the client to decrease feelings of insecurity. 2.Do not argue, bargain or try to reason with the client 3. Merely set the limits and expectations. 4. Help the client recognize that he must accept the consequences of own behaviors and refrain from attributing them to others. |
1. It facilitates the acceptance of the individual and his or her behavior. 2. Because of the strong id influence on client’s behavior he or she should receive immediate feedback when behavior is unacceptable. 3. He must accept responsibility for own behaviours before adaptive change can occur. |
|
|
4. Imbalanced nutrition less than body requirement related to decreased appetite evidenced by loss of weight and refusal to sit still long enough to eat. |
Short Term Goal: Client will consume sufficient food to meet recommended daily allowances of nutrients. Long Term Goals: Client will exhibit no signs or symptoms of malnutrition. |
1. Determine the client’s likes and dislikes. 2. Provide the client high protein and high calorie diet. 3. Weigh the client daily. 4. Maintain an accurate record of intake output and calorie count. 5. Sit with the client during meals. |
1. The client is more likely to eat foods that he or she particularly Enjoys 2. Nutritious intake is required on a regular basis to compensate for increased caloric requirements due to hyperactivity. 3. As it provides idea about weight gain. 4. It provides an objective assessment about the nutritional status. 5. To a ses whether the client takes food or not. |
|
|
5. Insomnia related to disease evidenced by sleeping only short periods. |
Short Term Goal: Within 3 days with the aid of a sleeping medication client will sleep 4-6 hrs. Without awakening. Long Term Goal: By time of discharge client will be able to acquire 6-8 hrs of uninterrupted sleep without medication. |
1. Monitor sleep pattern. Provide a structured schedule of activities that includes established times for naps or rest. 2. Avoid intake of caffeinated drinks such as tea, coffee and colas. 3. Advise the client to go for relaxation exercises, soft music and non-stimulating drinks. |
1. Accurate baseline data is important in planning care to help the client with this problem. 2. As caffeine is a CNS stimulant and may interfere with the client’s achievement of rest and sleep. 3. It promotes sleep. 4. To assist the client to achieve sleep until normal sleep is restired. |
Presentation of bipolar disorder
Manic
Depressed
Mixed
Types of bipolar disorder
TYPE I - manic/mixed episode +/- major depressive episode.
TYPE II - hypomanic episode + major depressive episode.
Cyclothymic disorder.
Other Bipolar disorders.
Bipoar disorder due to a general medical condition.[5]
Substance induced bipolar disorder.
Incidence and prevalence
Annual incidence 7 per 100,000 Estimated lifetime prevalence — bipolar 14–16 per 1000 Peak onsets between 15 and 19 years of age Suicide bipolar 1 — 17% attempt suicide, bipolar disorder — 0.4% die annually by suicide
Epidemology
Lifetime prevalence Type I — 0.7 – 0.8% Type II — 0.4 – 0.5% Equal in males and females Increased prevalence in upper socioeconomic classes Age of Onset.
Usually late adolescence or early adulthood. However, some after age 50. Late onset is more commonly Type II. a) Predisposing factors, b) Genetics.
Greater risk in first degree relatives (4-14 times risk).
Concordance in mono zygotic twins >85%.
Concordance in dizygotic twins — 20%.
Secondary causes of mania
Toxins.
Drugs of Abuse.
Stimulants (amphetamines, cocaine.
Hallucinogens (LCD, PCP).
Prescription Medications.
Common: antidepressants, L-dopa, corticosteroids.
Neurologic.
Nondominant frontal CVA, Nondominant frontal tumors, Huntington’s Disease and Multiple Sclerosis.
Infectious Neurosyphilis and HIV.
Endocrine: Hyperthyroidism and Cushing’s Disease.
Treatment
Education and Support.
Medication.
Acute mania: Lithium, Carbamazepine, Valproate, Lamotrigine, antipsychotics, benzodiazepines.[6]
Long Term Mood Stabilization: Lithium, Carbamazepine, Valproate, Lamotrigine, possibly atypical antipsychotics.
Comorbidity is common
Anxiety (30–50%) Substance misuse disorders (drugs[7] and alcohol) (30–50%) Personality disorders, in particular borderline personality disorder (exercise caution when diagnosing).
Health education given to patient
Client/family education regarding medications (anticonvulsants and antipsychotics)[8]
Refrain from discontinuing the drug abruptly.
Report the following symptoms to the physician immediately: Skin rash, unusual bleeding, spontaneous bruising, sore throat, fever, dark urine and yellow skin or eyes.
Not drive or operate dangerous machinery until the reaction to the medication has been established.
Avoid consuming alcoholic beverages and non-prescription medications without approval from physician
Carry card all the times identifying the names of medications being taken.
Use sun block lotion and wear protective clothing when spending time outdoors.
Rise slowly from a sitting or lying position to prevent a sudden drop in blood pressure.
Take frequent sips of water chew sugarless gum, or suck on hard candy if a dry mouth is a problem.
Consult the physician regarding smoking while on antipsychotic therapy.[9]
Continue to take the medication, even if feeling well and as though it is not needed. Symptoms may return if medication is discontinued.
Follow-up community care
Educated the patient regarding continuity of care and medication monitoring.
Activities of daily living
Many people with BPAD have serious cognitive deficits that affect their ability to function alone. These can include problems with short-term memory, planning, prioritizing, organization and decision-making. Provided the patient regarding basic life skills activities and cognitive remedial therapy.
Follow-up physical health care
As physical illness is higher among psychiatric patients than in the general population. Psychiatric symptoms can cause patients to neglect physical health problems, so follow-up care in the community is important for health maintenance and prevention. Including dental care and eye care.[10]
Source of Funding
None.
Conflict of Interest
The author declares that there is no conflict of interest.
References
- G. E. Berrios. Of Mania: Introduction. Hist of Psychiatry 2004. [Google Scholar] [Crossref]
- . The ICD-10 Classification of Mental and Behavioural Disorders. World Health Organization 2012. [Google Scholar]
- Lionel Robbins. Diagnostic and statistical manual of mental disorders: DSM-5. 2013. [Google Scholar]
- Dennis S. Charney, Kenneth L. Davis, Joseph T. Coyle. Neuropsychopharmacology. 2002. [Google Scholar]
- Bushra Mushtaq. Role of Psychiatry Nurse in Anti-Manic Drugs. Arch of Pharm& Pharmacol Res 2018. [Google Scholar] [Crossref]
- Omar Khan, Nagy A Youssef. A brief history of polarity in mood and its diagnostic evolution. Ann Clin Psychiatry 2018. [Google Scholar]
- . Drug Addiction and Adolescents. J Nurs & Care 2017. [Google Scholar] [Crossref]
- Bushra Mushtaq. Process Recording, a way of Therapeutic Communication Between a Nurse and Client with Psychiatric Illness. J Counselling and Fam Ther 2020. [Google Scholar] [Crossref]
- Javaid Ahmad Mir, Bushra Mushtaq. Crisis as psychiatric emergency and Role of psychiatric nurse. JONA J Nurs Administration 2018. [Google Scholar]
- Bushra Mushtaq, Javaid Ahmad Mir. Psychiatric rehabilitation. Drug Des, Dev and Ther. 2018. [Google Scholar]
